The CQC has told us they will carry out a formal “well-led” assessment over three days between Tuesday 10 April and Thursday 12 April 2018. They have already started unannounced visits and more will occur over the coming weeks and months. This is to help them ensure that the information gained from the visits can be included into the well-led research and preparation.
They only have to give us 30 minutes notice of a visit, so the message to all staff is be prepared for the CQC to visit, and organise your teams and services.
The CQC ask the same five questions of all the services they inspect. These are:
| Question | What this means for patients and the public |
| Are they safe? | You are protected from abuse and avoidable harm. |
| Are they effective? | Your care, treatment and support achieves good outcomes, helps you to maintain quality of life and is based on the best available evidence. |
| Are they caring? | Staff involve and treat you with compassion, kindness, dignity and respect. |
| Are they responsive to people’s needs? | Services are organised so that they meet your needs. |
| Are they well-led? | The leadership, management and governance of the organisation make sure it’s providing high-quality care that’s based around your individual needs, that it encourages learning and innovation, and that it promotes an open and fair culture. |
This inspection gives us an opportunity to shout about all the good things about ULHT and the progress we’ve made, as well as our plans to continue to improve.
Here is a list of some of the things we have done (I’m sure you’ll have more). See the intranet for a longer list.
- We have more consultants, more middle grade doctors, more allied health professionals and more non-registered nurses working at the Trust than 12 months ago.
- The number of patients waiting over 12 weeks for a first outpatient appointment has more than halved.
- Launched our 2021 roadmap including a new vision of “excellence in rural healthcare” and values.
- Launch of our staff charter and behavioural framework, which clearly lays out the expectations that the Trust has of its staff, and what staff should expect from the Trust.
- Launched a new freedom to speak up policy: voicing my concerns, highlighting five ways they can raise concerns. This includes promotion of our Trust’s Freedom to Speak Up Guardian, Jayne Warner.
- The “golden hour” introduced each day where heads of nursing and matrons set aside the time to do structured checks of the wards to see how we are providing care to patients, to ensure that each area of the hospital is providing the same high quality standard of care.
- Extensive work has been done on improving our health records in December 99% of records were available in clinics.
- Over 81% of our staff have had a flu vaccination this year- making us one of the top-performing trusts in the country.
- Every department across the Trust now has a sepsis box.
What we need you to do
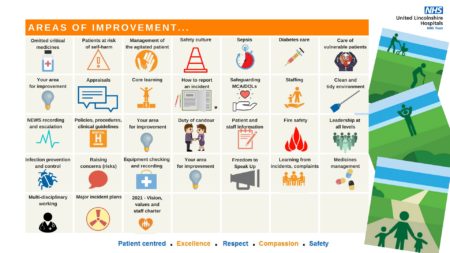
- Remind yourselves of the good work you’ve done and your priorities for improvement over the next 6 months by using your improvement calendar. Share these on twitter and Facebook using the #our2021improvements

Inspection readiness – top tips
As the CQC could turn up any day, here are some tips to prepare:
- No fixed date – start preparing now!
- Rosters and staffing – know your establishment and how to escalate issues (see video on safe staffing here)
- Learning from incidents and complaints – how does it happen?
- What were the last three incidents?
- What is the biggest risk in your area and are you mitigating it?
- How do you escalate risks/concerns and how do you get feedback?
- NEWS recording and escalating deteriorating patients.
- Improvement calendar – talking about improvements.
- Improvement walks – fresh pair of eyes peer review of wards/departments.
Inspection readiness – getting the basics right
Here are the basics that the CQC will want to see.
- Clean and tidy wards/clinical areas.
- Resus trollies, drug fridges and controlled drugs are checked.
- Equipment is PAT tested.
- Drug trollies and drug rooms are locked.
- COSHH substances are locked up.
- Hand hygiene is adhered to.
- Records check – e.g. assessments, fluids balance charts etc.
- DNACPR.
- Duty of candour is followed.
- Notice boards are up to date and tidy.
- Mandatory training and appraisals are up to date.
- MCA/DoLs and clinical holding/restraint.
